Literature Review of Syphilis Among Pregnant Women in Ethiopia Pdf
- Enquiry
- Open Access
- Published:
Sero-prevalence of syphilis and associated factors amid pregnant women in Ethiopia: a systematic review and meta-assay
Systematic Reviews volume 10, Article number:223 (2021) Cite this article
Abstract
Background
Syphilis remained a major cause of reproductive morbidity and poor pregnancy outcomes in developing countries. Previously, studies showed inconsistent results and failed to show the bodily picture of the diseases in Ethiopia. Thus, the aim of this meta-assay was, offset, to determine the updated pooled prevalence of syphilis amid pregnant women in Federal democratic republic of ethiopia and, second, to assess its associated factors.
Methods
A comprehensive search was made on PubMed, Google scholar, Science Direct, and African Journals Online databases to identify relevant manufactures. A random effects model was used to estimate pooled syphilis prevalence and odds ratio (OR) with the corresponding 95% confidence intervals (CIs) using STATA fourteen statistical software. I 2 statistics and Egger'south regression exam in conjunction with funnel plot was used to decide heterogeneity and publication bias among included studies respectively.
Effect
Nosotros identified xiii suitable studies in this analysis. Accordingly, the pooled prevalence of syphilis among pregnant women in Ethiopia was 2.32% (95% CI, 1.68–ii.97). Specifically, syphilis prevalence was 2.53% (95% CI, 1.92–3.fourteen%) and ane.xc% (95% CI, 0.xl–3.40%) as per the treponemal and non-ytreponemal diagnostic test, respectively. On the other hand, regional analysis indicated that 4.06% (95% CI, 2.86–v.26) in Southern Nations Nationalities and Peoples (SNNP), ii.sixteen% (95% CI, 1.57–2.75) in Amhara and 1.46% (95% CI, 0.69–2.23) in Oromia region. Being married (OR, 0.37 (95% CI, 0.12–0.91%)) was less probable to develop syphilis. On the other hand, women with history of multiple sexual partner (OR, two.98 (95% CI, i.15–7.seventy)) and women with history of previous sexually transmitted infection (STI) (OR, 4.88 (95% CI, ane.35–17.62)) have higher run a risk to develop syphilis. Besides, the pooled syphilis-HIV coinfection was 0.80% (95% CI, 0.60–ane.01%).
Decision
This study provides evidence of relatively high prevalence of syphilis among pregnant women in Ethiopia. Therefore, it is recommended to further ramping up of current intervention measures to prevent future generations.
Systematic review registration
PROSPERO CRD42020211650
Background
Syphilis is a sexually transmitted infection (STI) acquired past the spirochete Treponema pallidum, and it continues to be a main public health trouble worldwide [ane]. It spreads primarily through sexual contact and vertical transmission and can rarely exist spread through blood transfusion. Syphilis can be successfully controlled by effective public health measures due to the availability of a sound diagnostic test and effective and economical handling options [2]. Yet, if syphilis is left untreated, it can lead to devastating fetal outcomes [three].
Pregnant women are sexually active and are at adventure of STI, including syphilis [4]. Globally, 36 million people are infected with syphilis, out of which 2 million are pregnant women. More half of infected women transmit the infection to their babies resulting in adverse pregnancy outcomes including early fetal expiry, stillbirth, preterm nativity, low birth weight, neonatal death, and built infection in infants [five].
Syphilis remained a major cause of reproductive morbidity and poor pregnancy outcomes in developing countries [four]. In sub-Saharan Africa, syphilis sero-prevalence ranges from 4 to 15%, and can cause agin outcomes in 50–80% of pregnancies [6]. Ethiopia is among the top three sub-Saharan countries with the highest numbers of adverse pregnancy outcomes attributed to syphilis [vii]. Furthermore, studies take demonstrated that 21% children built-in from seropositive mothers in Ethiopia developed signs of syphilis. Likewise, stillbirth and abortion rates of syphilis diagnosed women were almost double relative to the general population [8].
Previously established systematic review and meta-analysis conducted on the prevalence of syphilis among pregnant women in Federal democratic republic of ethiopia includes only five studies with smaller sample size and did not report syphilis prevalence based on the diagnostic test modality. As well, it failed to demonstrate syphilis-HIV co-infection and predictors of syphilis sero-positivity [9]. Thus, in the absenteeism of concrete and inclusive evidence in STI endemic settings including HIV and syphilis, this systematic review and meta-analysis was conducted to determine the updated pooled prevalence of syphilis among meaning women in Ethiopia. Moreover, syphilis sero-reactivity associated factors and syphilis-HIV co-infection was also determined in this written report to guide public health intervention and control measures.
Methods and materials
Reporting and study protocol registration
This review was conducted according to the requirements of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [10] (Additional file 1). This study was registered in International Prospective Register of Systematic Reviews (PROSPERO) database with protocol number, CRD42020211650.
Search strategy and data sources
An inclusive literature search was made from September 1 to 30, 2020, on PubMed, Google scholar, Science Direct, and African Journals Online databases based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [10]. The following fundamental words were used for PubMed database searching: ["Syphilis" or "Treponema pallidum" AND (magnitude OR prevalence OR seroprevalance) AND "significant women" OR "pregnant" AND "Ethiopia"]. In improver, literatures and reference lists of relevant articles were also retrieved to find boosted studies.
Inclusion and exclusion criteria
All articles fulfilling the following weather were screened and later assessed for eligibility. Published studies conducted but in Ethiopia and reporting prevalence of syphilis amid pregnant women, published in English language upward to the end of September 2020. Studies with a clear clarification of participants' involved and state the number of participants tested for syphilis, and articles with a clear number and/or prevalence of syphilis cases were also considered. Yet, citations without abstracts and/or total-text, review articles, conference abstracts, editorials, duplicate studies, commentaries, trend analyses, studies which include non-pregnant women and those which exercise not report syphilis prevalence were excluded from the review. Similarly, given the known synergy between HIV and syphilis [11], studies conducted prior to HIV antiretroviral availability (before Jan 2005 in Federal democratic republic of ethiopia) [12] were also excluded as this would affect syphilis prevalence.
Issue of interest
The primary issue of this report was the prevalence of syphilis amidst significant women. Moreover, the results have been stratified by diagnostic examination (treponemal vs not-treponemal testing) and different geographical regions in Federal democratic republic of ethiopia. Secondly, nosotros have also determined factors associated with syphilis sero-positivity: marital condition (married vs non cohabiting; non cohabiting involves: unmarried, widowed, and divorced), previous STI (nowadays vs absent), and previous history of multiple sexual partner (present vs absent). In improver, the prevalence of syphilis-HIV co-infection was also adamant.
Study option, quality assessment, and data extraction
The championship and abstract of studies were screened after removing duplicates. Full-text review was conducted for manufactures constitute to be relevant by tittle and abstract to identify potential articles for inclusion in this meta-analysis.
The quality of included studies was evaluated past using Joanna Brigg's Plant (JBI) quality cess checklist for prevalence studies [thirteen]. Based on the JBI checklist, studies with a quality score of 50% and above were considered high quality and involved in the analysis. Extracted data includes the following descriptive data: writer and publication year, report area/region, study flow, laboratory methods employed to diagnose syphilis, sample size, and prevalence of syphilis. In addition, prevalence of syphilis by marital status, presence/absenteeism of previous history of multiple sexual partner, and history of previous STI were extracted whenever reported. Ii independent reviewers (HG and DG) were involved in study selection, quality assessment, and data extraction. Disagreement between the reviewers was solved by discussion.
Statistical methods and analysis
Information were entered into Microsoft Excel and then exported to STATA 14 statistical software for further analysis. The I ii values of 25, 50, and 75% was considered low, medium, and high heterogeneity, respectively [14]. In pooled prevalence analysis and 95% confidence intervals (CIs), the random effects model (DerSimonian-Laird method) [fifteen] was used. The overall and subgroup analysis of random furnishings model with 95% CIs were calculated and demonstrated using a forest plot. All the same, for studies with small (well-nigh 0) or large (near 1) prevalence, the inverse variance method was not stable and hence, we used Freeman Tukey arcsine methodology to address stabilizing variances as evidenced elsewhere [12, 16, 17]. Syphilis-HIV co-infection and the effect of selected predictor variables including marital status, previous history of multiple sexual partner, and previous history of STI on syphilis prevalence was analyzed using separate categories of meta-analysis.
The existence of publication bias was adamant using funnel plot and Egger's regression test. In Egger'south test, p < 0.05 was considered statistically significant [18]. The effect of each study on the overall pooled prevalence was determined past using sensitivity analysis. Sensitivity exam eliminates each written report step by step in the analysis to betoken the pooled effect sizes and related heterogeneity attributed by each private study.
Result
Study selection
A comprehensive combined literature search generated a full of 936 possible articles, of which xx were chosen sensibly for detailed full-text assessment and xiii studies were found to be appropriate for consideration in the meta-synthesis (Fig. 1).
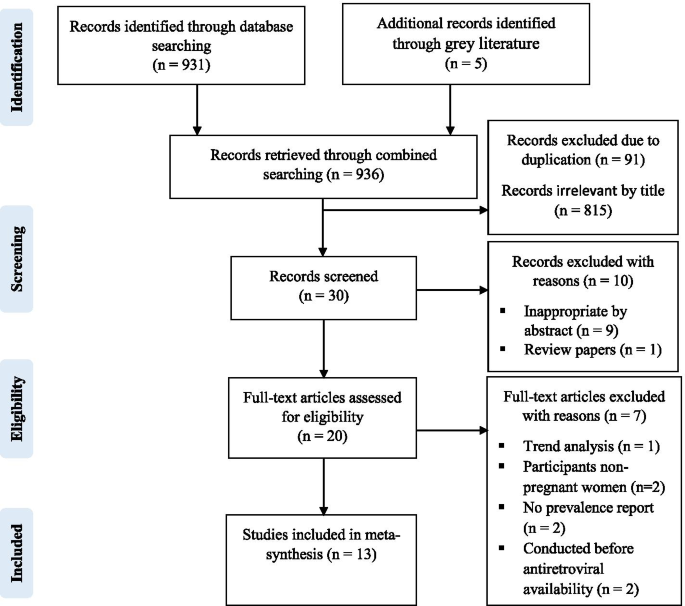
PRISMA flow chart for the studies screened, reviewed and included
Characteristics of included studies
Among the xiii studies [19,xx,21,22,23,24,25,26,27,28,29,thirty,31] included in the meta-analysis, a total of 17,656 meaning women were screened for syphilis in 3 different regions of Ethiopia. Regional distribution of studies revealed that eight [19,20,21,22,23,24, 26, 29] from Amhara, ii [25, 28] from Southern Nations Nationalities and Peoples (SNNP) and iii [27, xxx, 31] from Oromia region. In spite of that, there was no any written report from other regions of Federal democratic republic of ethiopia fulfilling the inclusion criteria. Except a single prospective cohort report [27] which was conducted in Assela, Oromia region; all included records were cross-sectional studies with study participants ranging from 181 [31] to 4346 [30] and conducted from 2005 to 2019. Different diagnostic tests were employed for screening syphilis; 6 studies [xix,20,21,22, 25, 31] used treponema pallidum hemagglutination assay (TPHA), three studies [24, 28, 29] used venereal diseases research laboratory (VDRL), two studies [26, xxx] employed rapid plasma reagin (RPR) test, and 1 study [27] used syphilis rapid immunoassay, while the other one [23] used Immuno-chromatography test strips (ICS test). As per the established literature, the TPHA, syphilis rapid immunoassay and ICS test constitute the treponemal test while the VDRL and RPR are non-treponemal diagnostic tests [32].
Out of 17,656 meaning women screened for syphilis, 416 were found positive. Out of 416 seropositive women, 172 were from SNNP, 183 were from Amhara, and 61 were from Oromia (Table 1).
Prevalence of syphilis among meaning women
The pooled prevalence of syphilis amid pregnant women in Federal democratic republic of ethiopia from the random effects model was 2.32% (95% CI, 1.68–2.97; I 2 = 98.9%; Eggers examination, p = 0.14). Subgroup analysis based on the diagnostic test employed indicated that ii.53% (95% CI, ane.92–3.14%) and 1.90% (95% CI, 0.forty–iii.twoscore%) syphilis prevalence using treponemal and non-treponemal test, respectively (Fig. 2). As graphically demonstrated in the symmetrical funnel plot, at that place was no prove of publication bias within included studies (Fig. 3). Moreover, this was too bodacious by Egger'south test (p = 0.14). In addition, the sensitivity analysis clearly indicated that the influence of individual studies on the summary result judge was not significant. Consequently, the pooled effect size guess of syphilis among pregnant women in Ethiopia was steady and reliable when analyzed past omitting one report at a time (Table 2).
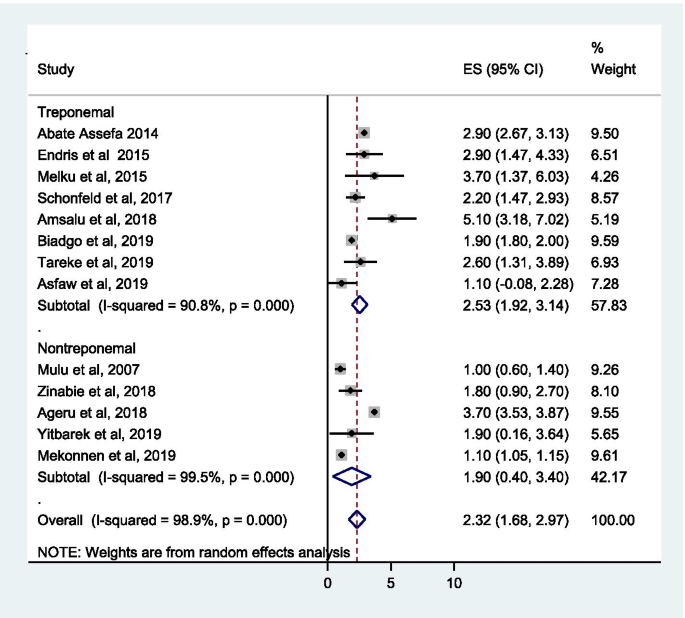
Pooled prevalence approximate (ES) of syphilis amidst significant women in Federal democratic republic of ethiopia
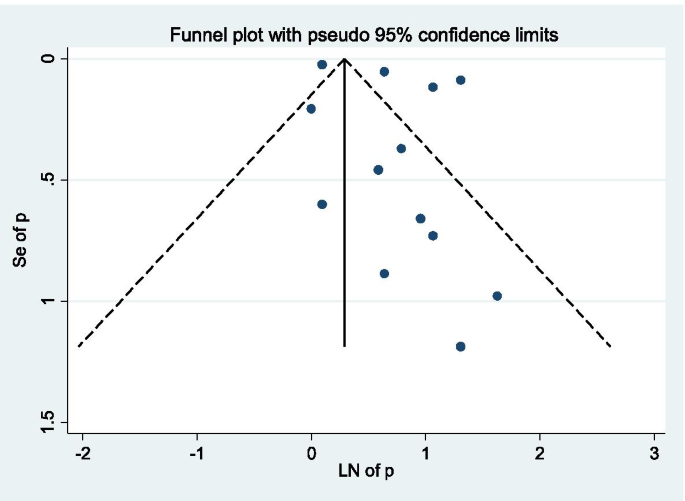
Funnel plot, evaluating the existence of publication bias for pooled syphilis prevalence
Syphilis prevalence in different regions of Federal democratic republic of ethiopia
The prevalence of syphilis based on the geographical regions of Ethiopia was 4.06% (95% CI, two.86–v.26) in SNNP, 2.16% (95% CI, 1.57–2.75) in Amhara, and 1.46% (95% CI, 0.69–2.23) in Oromia region (Table 3).
Pooled prevalence of syphilis-HIV co-infection amidst pregnant women
The overall pooled prevalence of syphilis-HIV co-infection among pregnant women in this meta-analysis was 0.80% (95% CI, 0.60–ane.01; I ii = 95.2%) (Fig. 4).
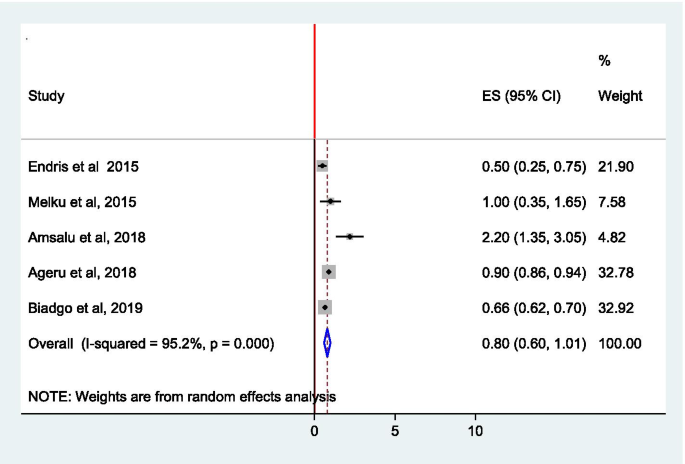
Pooled prevalence guess (ES) of syphilis-HIV co-infection amidst pregnant women in Ethiopia
Factors associated with syphilis sero-positivity
The association of syphilis sero-positivity with marital condition, previous history of multiple sexual partner and previous history of STI was quantified using OR. The odds of having syphilis are virtually three times higher in meaning women who had history of multiple sexual partners than those who had no such partner, OR ii.98 (95% CI, 1.15–7.70). Pregnant women who had previous history of STI were more than four times more likely to develop syphilis than women who had no such history, OR 4.88 (95% CI, ane.35–17.62), whereas married women had 63% lower take a chance of having syphilis compared to those who are non cohabiting (single, widowed, divorced), OR 0.37 (95% CI, 0.12–0.91) (Table 4).
Discussion
Syphilis is one of the easily preventable and treatable sexually transmitted infections only continued to exert a high brunt worldwide especially in sub-Saharan Africa where resources are scarce. Therefore, prevention and command of syphilis among pregnant women using advisable intervention measures is crucial for the emergence of syphilis free generation. For that, determining the actual burden of syphilis infection and antenatal care (ANC) follow-up screening plays a great role in early diagnosing and treatment of syphilis, and prevention of its vertical manual. This study aimed to determine the updated pooled prevalence and factors associated to syphilis positivity, and the pooled syphilis-HIV co-infection amongst pregnant women in Ethiopia.
This meta-analysis showed that the overall pooled prevalence of syphilis amidst pregnant women in Ethiopia was ii.32% (95% CI, 1.68–2.97). The pooled prevalence was two times higher than the recent nationwide HIV/syphilis watch reports amidst ANC attendees in Federal democratic republic of ethiopia (ane.i%) [33]. The variation in syphilis prevalence between this meta-assay and the sentinel survey might be due to the rough estimate nature of the sentinel report that might underrepresent the actual burden of the diseases. Contrastingly, previous meta-analysis reported higher prevalence of syphilis amongst pregnant women in Ethiopia, 3.67% [9] relative to this study. This might be because of the previous meta-assay includes studies with higher syphilis prevalence conducted in the pre-antiretroviral therapy availability. Yet, given the known synergy between HIV and syphilis [11], nosotros take excluded studies conducted prior to HIV antiretroviral availability in this meta-analysis. Also, the diseases dynamics may change overtime and impact the observed prevalence [34]. Partly, it may be due to the difference in the number of included studies (5 studies in earlier meta-assay and 13 articles in this report), indicating the sample size may impact the prevalence.
On the other hand, the pooled prevalence in this meta-analysis was comparable with the study from a countrywide surveillance of HIV/syphilis prevalence among pregnant women attending ANC in Tanzania (2.v%) [35]. The similarity in syphilis prevalence in Ethiopia and Tanzania might exist partly due to the WHO'due south increased focus and prioritization of antenatal syphilis (in conjunction with HIV and hepatitis B virus) screening for better intervention measures. Besides, combination rapid HIV/syphilis tests are at present used to a greater degree in ANC which may also upshot in increased syphilis testing/diagnoses in different countries of the world to betoken the actual moving picture of the diseases in diverse settings.
As shown in subgroup analysis, this written report indicated relatively higher prevalence of syphilis using treponemal diagnostic test modality ii.53% (95% CI, 1.92–3.fourteen%) compared to the non-treponemal exam 1.90% (95% CI, 0.40–3.40%). This could be due to reactivity to a treponemal test implies infection but it does non make up one's mind whether the infection is recent or remote or whether information technology has been treated or not [32]. Thus, it suggests that treponemal tests stay positive for decades after handling and may not always indicate active infection. On the other mitt, non-treponemal tests accept a high faux-positive rate and are hard to interpret on their own [32]. Therefore, considering the difficulty of syphilis diagnosis, the results have to be interpreted with care.
Regional analysis showed a higher and lower prevalence of syphilis in SNNP (iv.06%) and in Oromia (1.46%) respectively. Higher syphilis prevalence in SNNP might be attributed to the risky socio-cultural practices such as polygamy is more good in SNNP [36] relative to other regions of Ethiopia. Partly, information technology might be due to the difference in the number of studies included in each category.
In addition, pooled gauge of syphilis-HIV co-infection was also assessed. Consequently, the overall pooled prevalence was 0.eighty% (95% CI, 0.60–1.01%). A comparable result (0.73%) was obtained from Commonwealth of Congo [37]. While a study in Tanzania reported lower (0.3%) prevalence [35], some other study from Rwanda indicated higher (1.2%) prevalence [38] of syphilis-HIV co-infection relative to the findings of this written report. The divergence in prevalence of syphilis-HIV co-infection might be attributed to the variation in level of implementation and integration of STI prevention and command measures in different countries.
Too, the clan between pregnant women with and without previous history of multiple sexual partner and syphilis sero-positivity was measured in this study. Appropriately, pregnant women with previous history of multiple sexual partners were 2.98 times more probable to get syphilis infection compared to women without such partner. This was consistent with previously established evidences [39,xl,41,42] and could be attributed to the fact that people with multiple sexual partner has higher risk of getting STI including syphilis. This report also showed that pregnant women with previous history of STI were iv.88 times at higher risk of developing syphilis relative to significant women without such history. This is in line with the findings from Malawi [43] and China [44]; this could be partly due to lack of behavioral change and other prevention interventions that resulted in maintaining risky behaviors among women who had history of previous STI.
On the other hand, this meta-analysis also demonstrated that married women had 63% lower risk of developing syphilis compared to those who are not cohabiting (unmarried, widowed, divorced). This was comparable with earlier studies conducted in rural Tanzania [45] and three sub-Saharan countries [46]. This might exist due to the tendency of not-cohabiting women to practice high-risk sexual behaviors similar having multiple sexual partners. Partly, this could be considering of women in ANC are sexually active age groups, suggesting that if they are non-cohabiting they may have high-chance sexual behaviors.
Limitations
Given the difficulty of syphilis diagnosis, most of the included studies used treponemal diagnostic test alone which may bear upon the prevalence report. Some regions in the country were non represented in this study due to lack of established original studies in the expanse. Furthermore, all included studies were facility based. Thus, estimation of findings has to exist with due consideration of these limitations.
Conclusions
This review provides evidence of relatively loftier prevalence of syphilis amidst pregnant women. This written report as well assessed the burden of syphilis-HIV co-infection and determinants of syphilis sero-reactivity in Ethiopia. Therefore, it is recommended to farther ramping upwards of current intervention measures, like routine screening of all ANC women and integration of syphilis testing and treatment to the already established HIV prevention program in the country. Farther, nationwide studies involving all regions are needed to assess the magnitude and determinant factors for syphilis among significant women in Federal democratic republic of ethiopia.
Availability of data and materials
Whatsoever data related to this manuscript will be accessible by requesting the corresponding author.
Abbreviations
- ANC:
-
Antenatal intendance
- CI:
-
Confidence interval
- HIV:
-
Homo immunodeficiency virus
- ICS examination:
-
Immuno-chromatography test
- OR:
-
Odds ratio
- RPR:
-
Rapid plasma reagin
- SNNP:
-
Southern Nations Nationalities and Peoples of Federal democratic republic of ethiopia
- STI:
-
Sexually transmitted infection
- TPHA:
-
Treponema pallidum hemagglutination assay
- VDRL:
-
Venereal diseases research laboratory
References
-
Kojima N, Klausner JD. An update on the global epidemiology of syphilis. Curr Epidemiol Rep. 2018;5(ane):24–38.
-
Khan S, Menezes GA, Dhodapkar R, Harish BN. Seroprevalence of syphilis in patients attending a tertiary care infirmary in Southern India. Asian Pac J Trop Biomed. 2014;4(12):995–7.
-
Peeling RW, Hook EW III. The pathogenesis of syphilis: the Neat Mimicker, revisited. J Pathol. 2006;208(2):224–32.
-
Tiruneh Yard. Seroprevalence of multiple sexually transmitted infections amongst antenatal clinic attendees in Gondar Health Center Northwest Federal democratic republic of ethiopia. Ethiopian Med J. 2008;46(four):359–66.
-
Organization WH. The global elimination of congenital syphilis: rationale and strategy for activeness. 2007.
-
Gloyd S, Chai Southward, Mercer MA. Antenatal syphilis in sub-Saharan Africa: missed opportunities for mortality reduction. Wellness Policy Plan. 2001;sixteen(1):29–34.
-
Kuznik A, Habib AG, Manabe YC, Lamorde M. Estimating the public health burden associated with adverse pregnancy outcomes resulting from syphilis infection across 43 countries in sub-Saharan Africa. Sex Transm Dis. 2015;42(7):369.
-
Naeye R, Tafari N, Marboe C, Judge D. Causes of perinatal mortality in an African city. Balderdash Earth Health Organ. 1977;55(one):63.
-
Tesfaye B: Gestational syphilis in Federal democratic republic of ethiopia, meta-assay and systemic review. In: 30th EPHA Annual Briefing: 2019;2019.
-
Moher D, Liberati A, Tetzlaff J, Altman DG, Grouping P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA argument. PLoS Med. 2009;6(7):e1000097.
-
Kenyon CR, Osbak One thousand, Chico RM. What underpins the refuse in syphilis in Southern and Eastern Africa? An exploratory ecological analysis. Int J Infect Dis. 2014;29:54–61.
-
Geremew D, Endalamaw A, Negash M, Eshetie S, Tessema B. The protective consequence of isoniazid preventive therapy on tuberculosis incidence among HIV positive patients receiving Fine art in Ethiopian settings: a meta-analysis. BMC Infect Dis. 2019;nineteen(ane):1–nine.
-
JB I. The Joanna Briggs Establish critical appraisal tools for use in JBI systematic reviews checklist for prevalence studies. North Adelaide: The Joanna Briggs Institute; 2017.
-
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-assay: Q statistic or I2 alphabetize? Psychol Methods. 2006;11(2):193.
-
DerSimonian R, Laird Northward. Meta-analysis in clinical trials. Control Clin Trials. 1986;vii(iii):177–88.
-
Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders amongst the homeless in western countries: systematic review and meta-regression assay. PLoS Med. 2008;5(12):e225.
-
Geremew D, Melku M, Endalamaw A, Woldu B, Fasil A, Negash Yard, Baynes HW, Geremew H, Teklu T, Deressa T. Tuberculosis and its clan with CD4+ T jail cell count amidst adult HIV positive patients in Ethiopian settings: a systematic review and meta-analysis. BMC Infect Dis. 2020;20:1–10.
-
Sterne JA, Egger M, Smith GD. Investigating and dealing with publication and other biases in meta-analysis. BMJ (Clinical inquiry ed). 2001;323(7304):101–5.
-
Assefa A. A iii year retrospective study on seroprevalence of syphilis among pregnant women at Gondar University Educational activity Hospital Ethiopia. Afr Health Sci. 2014;xiv(1):119–24.
-
Biadgo B, Hassen A, Getaneh M, Tesfa H, Jaleta KN, Eshetu T, Kasew D, Melku M. Syphilis and human immunodeficiency virus infections amid pregnant women attention antenatal care clinic of Gondar family guidance association, Northwest Ethiopia: implication for prevention of female parent to kid transmission. Reprod Wellness. 2019;16(ane):27.
-
Endris K, Deressa T, Belyhun Y, Moges F. Seroprevalence of syphilis and homo immunodeficiency virus infections amid pregnant women who attend the University of Gondar teaching hospital, Northwest Ethiopia: a cross sectional report. BMC Infect Dis. 2015;15:111.
-
Melku Grand, Kebede A, Addis Z. Magnitude of HIV and syphilis seroprevalence among pregnant women in Gondar, Northwest Ethiopia: a cross-sectional study. HIV/AIDS (Auckland, NZ). 2015;7:175–82.
-
Tareke K, Munshea A, Nibret E. Seroprevalence of syphilis and its adventure factors amongst pregnant women attention antenatal care at Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia: a cross-sectional written report. BMC Res Notes. 2019;12(1):69.
-
YidegYitbarek M, Ayele BA. Prevalence of syphilis among pregnant women attending antenatal intendance clinic, Sede Muja District, South Gondar, Northwest Federal democratic republic of ethiopia. J Pregnancy. 2019;2019:1584527.
-
Amsalu A, Ferede G, Assegu D. Loftier seroprevalence of syphilis infection among meaning women in Yiregalem infirmary southern Ethiopia. BMC Infect Dis. 2018;18(one):109.
-
Mulu A, Kassu A, Tessema B, Yismaw G, Tiruneh M, Moges F, Wondmikun Y, Nishikawa T, Ota F. Seroprevalence of syphilis and HIV-1 during pregnancy in a teaching infirmary in northwest Ethiopia. Jpn J Infect Dis. 2007;60(4):193.
-
Schönfeld A, Feldt T, Tufa TB, Orth HM, Fuchs A, Mesfun MG, Pfäfflin F, Nordmann T, Breuer M, Hampl One thousand, et al. Prevalence and impact of sexually transmitted infections in pregnant women in key Ethiopia. Int J STD AIDS. 2017;0(0):1–8.
-
Ageru TA, Abiso TL. Sero-prevalence of HIV and syphilis infection among significant mothers attended labor ward at Wolaita Sodo Academy Pedagogy Referral Hospital: a five-year retrospective written report (2012–2016). Am J Health Res. 2018;6(3):67–73.
-
Zinabie S, Belachew E, Yidenek T, Lewetegn M, Asfaw T. Sero-prevalence of syphilis and HIV and associated factors in pregnant women attending antenatal care clinics in Debre Berhan Public Wellness Institutions, Ethiopia. Am J Biomed Life Sci. 2018;6(3):56–62.
-
Wubete M, Mohammed M, Mengistu M, Mekonnen R: Prevalence of syphilis amid pregnant women attending antenatal dispensary of Bulchana Health Center, Shashemene, Westward Arsi Zone, Ethiopia. Int J Med Biomed Stud. 2019;iii(2). https://www.semanticscholar.org/paper/PREVALENCE-OF-SYPHILIS-AMONG-PREGNANT-WOMEN-Clinic-Wubete-Mohammed/7115c1b8f8b4498198653a6776f9b4458c33c309.
-
Fikadu B, Gebrish S, Asfaw T. Sero-prevalence of syphilis amidst pregnant women attending Antenatal Care Clinic at Jimma Univeristy specialized Hospital, Ethiopia. J Med Medical Sci. 2019;x(1):1–5.
-
Henao-Martínez AF, Johnson SC. Diagnostic tests for syphilis: new tests and new algorithms. Neurology. 2014;4(2):114–22.
-
Ababa A: Report on the 2014 round antenatal care based sentinel HIV surveillance in Ethiopia. Ethiop Public Heal Instititute 2015. https://ephi.gov.et/wp-content/uploads/2014/09/2014roundANCbasedHIVsurveillancereport.pdf.
-
Korenromp EL, Mahiané SG, Nagelkerke N, Taylor MM, Williams R, Chico RM, Pretorius C, Abu-Raddad LJ, Rowley J. Syphilis prevalence trends in developed women in 132 countries–estimations using the spectrum sexually transmitted infections model. Sci Rep. 2018;8(1):1–x.
-
Manyahi J, Jullu BS, Abuya MI, Juma J, Ndayongeje J, Kilama B, Sambu V, Nondi J, Rabiel B, Somi G. Prevalence of HIV and syphilis infections amid pregnant women attending antenatal clinics in Tanzania, 2011. BMC Public Health. 2015;15(1):501.
-
Tesfay GH. Note on: the adverse effects of polygamy on the rights of women: a case report in Gedeo and Sidama Zones. Haramaya Law Rev. 2017;vi:91–110.
-
Niama RF, Bongolo NCL, Kombo ESB, Yengo R, Mayengue PI, Kosso E-BM, Louzolo I, Macosso Fifty, Dzeret G, Babeaux ASPD: Syphilis and HIV infections amongst pregnant women attending antenatal clinics in Republic of Congo. Pan Afr Med J 2017;28(one). https://world wide web.ncbi.nlm.nih.gov/pmc/articles/PMC5681004/.
-
Françoise Northward, Bosco MJ, Bellancille N, Théoneste N. HIV/AIDS and syphilis sero-prevalence among pregnant women attending antenatal care eye in Rwanda. Am J Lab Med. 2020;5(4):83.
-
Yahya-Malima KI, Evjen-Olsen B, Matee MI, Fylkesnes K, Haarr Fifty. HIV-1, HSV-2 and syphilis among pregnant women in a rural area of Tanzania: prevalence and take chances factors. BMC Infect Dis. 2008;8(i):75.
-
Mutagoma Thousand, Remera East, Sebuhoro D, Kanters S, Riedel DJ, Nsanzimana S: The prevalence of syphilis infection and its associated factors in the full general population of Rwanda: a national household-based survey. J Sexually Transmitted Dis 2016;2016. https://world wide web.hindawi.com/journals/jstd/2016/4980417/.
-
Macêdo VCd, Lira PICd, Frias PGd, Romaguera LMD, Caires SdFF, Ximenes RAdA. Risk factors for syphilis in women: example-control written report. Rev Saude Publica. 2017;51:78.
-
Sombie I, Meda N, Cartoux K, Tiendrebeogo Southward, Ouangre A, Yaro S, Ky-Zerbo O, Dao B, Van de Perre P, Mandelbrot L. Seroprevalence of syphilis amongst women attending urban antenatal clinics in Burkina Faso, 1995–viii. Sexually Transm Infect. 2000;76(4):314–6.
-
Kwiek JJ, Mwapasa V, Alker AP, Muula AS, Misiri HE, Molyneux ME, Rogerson SJ, Behets FM, Meshnick SR. Socio-demographic characteristics associated with HIV and syphilis seroreactivity among pregnant women in Blantyre, Malawi, 2000–2004. Republic of malaŵi Med J. 2008;20(iii):80–5.
-
Zhou H, Chen XS, Hong FC, Pan P, Yang F, Cai YM, Yin YP, Peeling RW, Mabey D. Risk factors for syphilis infection amongst pregnant women: results of a case-control report in Shenzhen Prc. Sex Transm Infect. 2007;83(half dozen):476–lxxx.
-
Todd J, Munguti Grand, Grosskurth H, Mngara J, Changalucha J, Mayaud P, Mosha F, Gavyole A, Mabey D, Hayes R. Risk factors for active syphilis and TPHA seroconversion in a rural African population. Sexually Transm Infect. 2001;77(ane):37–45.
-
Potter D, Goldenberg RL, Read JS, Wang J, Hoffman IF, Saathoff E, Kafulafula G, Aboud S, Martinson Atomic number 26, Dahab G. Correlates of syphilis seroreactivity amidst pregnant women: the HIVNET 024 Trial in Malawi, Tanzania, and Zambia. Sexual activity Transm Dis. 2006;33(10):604.
Acknowledgements
We thank the authors of individual studies included in this meta-analysis.
Author data
Affiliations
Contributions
HG and DG: Conceived and designed the study, reviewed literatures, extracted and analyzed data, interpreted results, and drafted the manuscript. Both authors take read and canonical the final manuscript.
Corresponding author
Ethics declarations
Ethics blessing and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no that they have competing interests.
Boosted information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, accommodation, distribution and reproduction in any medium or format, as long as yous give advisable credit to the original writer(s) and the source, provide a link to the Creative Eatables licence, and signal if changes were made. The images or other third party material in this commodity are included in the commodity'due south Artistic Eatables licence, unless indicated otherwise in a credit line to the material. If fabric is not included in the article's Creative Eatables licence and your intended use is not permitted by statutory regulation or exceeds the permitted apply, y'all will need to obtain permission direct from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made bachelor in this article, unless otherwise stated in a credit line to the information.
Reprints and Permissions
Well-nigh this commodity
Cite this article
Geremew, H., Geremew, D. Sero-prevalence of syphilis and associated factors amongst pregnant women in Ethiopia: a systematic review and meta-analysis. Syst Rev ten, 223 (2021). https://doi.org/10.1186/s13643-021-01786-3
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s13643-021-01786-3
Keywords
- Syphilis
- Aero-prevalence
- Pregnant women
- Meta-analysis
- Ethiopia
Source: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01786-3
0 Response to "Literature Review of Syphilis Among Pregnant Women in Ethiopia Pdf"
إرسال تعليق